Radiology – the future of diagnosis and treatment | The News Tribe Blogs
The
international imaging community is organizing International Day of Radiology
(IDoR) on Thursday 8th November 2012 to raise awareness of the value
of radiology to safe patient care, and to improve understanding of the vital
role of radiologists in the healthcare practice. The purpose of this day is to increase
knowledge of radiographic imaging and therapy, which play a crucial role in
diagnosis and treatment of patients. World Radiology Day marks the anniversary
of the discovery of X-rays in 1895, on this day Professor Wilhelm Roentgen
discovered X-rays and within three months of discovery radiographs were
generated in major cities. In honor of his discovery, the European Society of
Radiology (ESR) along with the Radiological Society of North America (RSNA) and
American College of Radiology (ACR) decided 8th November should be
marked yearly with a devoted day of observance.
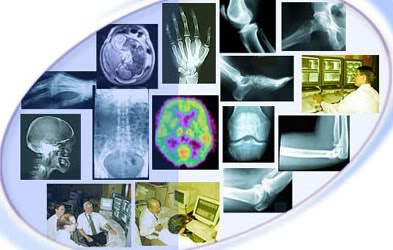
Medical
imaging is one of the most thrilling and progressive discipline in healthcare
and a field of great activities in terms of technological and biological
research. Early radiology was embedded in morphology, namely skeletal
morphology. The change towards image of physiology of the human body began with
radiology and nuclear medicine. In the midst of the excitement brought about by
the Roentgen’s discovery, Becquerel discovered radioactivity in the early 1896.
Similar to the discovery of x-rays, phosphorescence was accidental thus, began
the dawn of the medical imaging age. Subsequently, numerous scientists for
instance Curies and Rutherford had contributed to the advancement of radiology.
Thus, the use of single-photon emission computed tomography (SPECT) and to a
greater extent positron emission tomography (PET) to display functional
abnormalities not detected by other imaging tools have made assessment of
treatment practicable.
In
the early years, radiographs were initially made onto glass photographic plates
which were coated with emulsion only on one side. In 1918, Eastman introduced
film coated with emulsion on two surfaces. Radiograph at this time was focused
on imaging of extremities, mainly to detect fractures and to localize position
of bullets. Further development brought about an intravenous contrast agent
marketed for urinary tract radiograph in 1927. The next development involved
the use of fluorescent screen, an x-ray tube, and x-ray table and red goggles
and required the radiologist to stare directly into the screen so that x-ray
images could be displayed in real time. This was a rather primitive method as
the fluorescence emitted was very dim. The iodine-based contrast arteriogram in
a patient was reported in 1929 by Dos Santos, more or less 34 years after the
discovery of x-ray. In the late 1980’s and early 1990’s however, two essential
technologies have greatly impacted the evolution of angiography; moveable
multiple-angle C-arm fluoroscopy and digital image acquisition. By the 1970’s
ultrasound (US) and computed tomography (CT) had arrived displacing angiography
as the supreme imaging tool in radiology. By the 1990’s duplex ultrasound, CT
angiography and Magnetic Resonance (MR) angiography began to replace diagnostic
arteriography for the direct study of vascular pathology. In most radiology departments
today, catheter-based angiography is reserved mainly for diagnosis of
atherosclerotic vessels and as an adjunct to interventional procedure. The
emergence of three powerhouses imaging tools namely ultrasound, computed
tomography and magnetic resonance imaging have revolutionized the care of
patients across the continuum of medicine and surgery.
Radiology
is now often referred to as ‘imaging’ reflecting the fact that it is no longer
dependant on x-rays alone. Over the years, ultrasound has stood the test of
time proving to be a safe, reliable, portable and cheap imaging modality. In
1972 the cross-sectional imaging became a catch phrase; this was attributed to
the invention of computed tomography. The earliest CT scanners were limited to
imaging of the head, by 1976 the technology had evolved to whole body scanners,
and by the 1980’s CT Scans had gained worldwide acceptance. Today there are an
estimated 600,000 locations around the world where this diagnostic tool is in
use. The prototype CT Scanners took roughly four minutes of lapsed time to
acquire a single image. Currently, modern units produce images in less than 0.5
seconds. The advent of CT had an enormous effect on our ability to ‘SEE’ inside
the body and immediately changed the practice of medicine; the momentum created
by CT scanners fueled the commercial development of MRI systems. In its
infancy, many thought that MRI would have a limited impact because of its high
cost, the technical difficulties associated with it and the belief the CT
scanning was a superior method of imaging. MRI has quickly become the primary
imaging method for brain and spine imaging as well as functional imaging of the
heart.
Computers
and the digital world have impacted the science of Radiology bringing it to what
it is today. The advancement of artificial intelligence in the last 25 years
has created an explosion of diagnostic imaging technique. These techniques have
now been developed for digital rather than photographic recording of
conventional radiographs. In the early days, a head X-ray would require up to
11 minutes of exposure time but now digital radiographic images are made in
milliseconds while reducing the radiation dose to as little as 2% of what was
used for the 11 minutes head examination 10 years ago. The resolution
achievable by the different imaging methods may be classified as spatial,
contrast or temporal. Spatial resolution is the ability of a system to resolved
anatomic detail. Contrast resolution is the ability of the system to
differentiate different tissue especially to distinguished normal from
pathological tissue. Temporal resolution is the ability of the modality to
reflect either changing physiological events such as cardiac motion or disease
remission or progression as a function of time. Each imaging modality has its
strength and weaknesses much to frustration of hospital administrators no
single method will solve all diagnostic problems and the fusion of knowledge
gleaned from different modalities would serve our patient best.


No comments:
Post a Comment